Some people in a coma seem to be able to imagine themselves swimming or walking
KENZO TRIBOUILLARD/AFP via Getty Images
One in five people in a coma may be “locked in”, meaning they are aware of their surroundings but unable to communicate. A large study has found that some people with severe brain damage can carry out complex mental tasks when instructed, despite not being able to move or speak.
It was easier to discount the phenomenon “when it was thought to be a rare occurrence”, says Nicholas Schiff at Weill Cornell Medical College in New York. But now, given the latest study, “no one can ignore it”.
People with so-called disorders of consciousness are either in a coma or a vegetative state, where they show no awareness of their environment, or a minimally conscious state, where they show occasional signs of arousal, such as opening their eyes, but minimal awareness. In 2019, researchers discovered that 1 in 10 of these individuals may be locked in.
To find out if doctors were missing people in this state, Schiff and his colleagues carried out behavioural and brain imaging tests on 353 people with severe brain damage over eight years at six international centres.
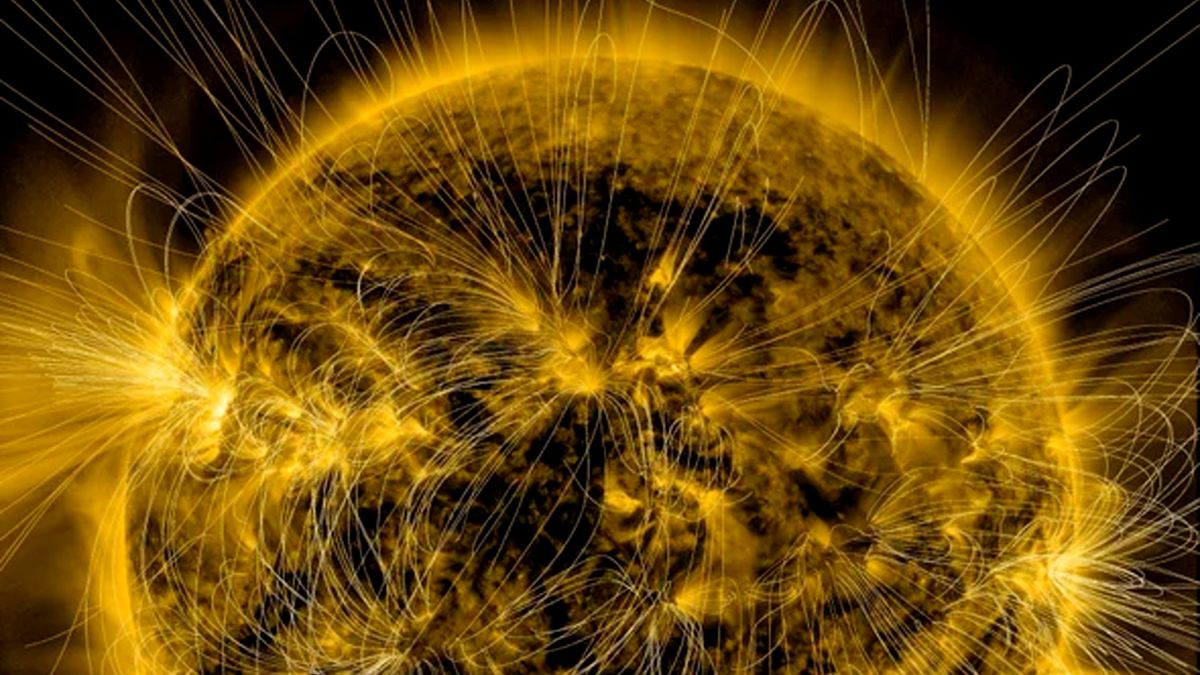
The participants were asked to think about performing a range of activities – such as playing tennis, swimming, clenching their fist or walking around their home – for 15 to 30 seconds, before pausing, and thinking about the activity again. This was repeated seven times over 5 minutes.
In people without disorders of consciousness, these thoughts produce distinct brain activity that can be identified using MRI scans or electroencephalograms (EEG). Among the 353 people with brain damage, 241 showed no outward response to verbal commands. But of these, 25 per cent showed brain activity that matched that of volunteers without brain damage. For those in a coma or a vegetative state specifically, the figure was 20 per cent.
“These are very demanding tasks – try thinking about swimming on and off for 5 minutes,” says Schiff. “We don’t know exactly what they are experiencing, but the fact that they can do this means there’s a very good chance that they have awareness.”
Estimates suggest that there are between 300,000 and 400,000 people with a prolonged disorder of consciousness worldwide, says Schiff, meaning up to 100,000 could have hidden awareness.
This study is of immense importance, says Raanan Gillon, emeritus professor of medical ethics at Imperial College London. For many people, the prospect of being kept alive in a non-conscious state is at best futile and at worst abhorrent, he says. “If, however, there is a significant probability that the lack of consciousness is only apparent, as these studies suggest may be the case, it can be anticipated that more people would wish to be kept alive and be consulted about their wishes before decisions are taken to discontinue life-prolonging treatment.”
Several ethical issues, including respect for people’s autonomy and their human rights “all require re-evaluation in light of these studies”, he says.
The results also raise questions on equitability regarding MRI and EEG access, says Erin Paquette at Northwestern University in Illinois. “If non-specialised centres don’t have access to these technologies, then patients in those centres may not have the same opportunities as others to change the course of their life.”
Brain-computer interfaces (BCI) could provide a way of giving people with consciousness disorders two-way communication, but aren’t commonly used in this group, says Schiff. A recent study showed it can take only 30 minutes to train a BCI to transform brain activity associated with attempted speech into text on a screen.
“Why not give them to those with a disorder of consciousness to see if they can use it to communicate?” says Schiff. “At worst you get two weeks of useful data, at best you free them.”
Topics:



















Discussion about this post