When the original Omicron variant swept across the country this winter, it launched America into a new COVID era, one in which nearly everyone—95 percent of adults, according to one CDC estimate—has some immunity to the virus through vaccines, infection, or both. Since then, however, Omicron subvariants have still managed to cause big waves of infection. They’ve accomplished this by eroding our existing immunity.
This will keep happening. “There’s not a lot of things I’m confident about in SARS-CoV-2 evolution, but I think I’m extremely confident we’ll keep seeing new variants that are progressively eroding antibody neutralization,” says Jesse Bloom, an evolutionary virologist at the Fred Hutchinson Cancer Center. Experts are cautiously optimistic that the pace of variant emergence will eventually slow, and for many people, reinfections are already milder and hospitals are not overwhelmed. But as the virus keeps changing, the only real guarantee is that it will be different—and that its changes won’t necessarily affect everyone uniformly.
SARS-CoV-2’s evolution follows a well-understood dynamic: When a variant sweeps around the world, it leaves behind a lot of immunity against itself. This puts intense evolutionary pressure on the virus to change things up; any subsequent variant has to somehow evade immunity to previous variants to keep finding new hosts. There are no limits to how long the coronavirus can keep doing this. Long-established respiratory viruses that cause the flu and common cold are still evolving to keep reinfecting us again and again.
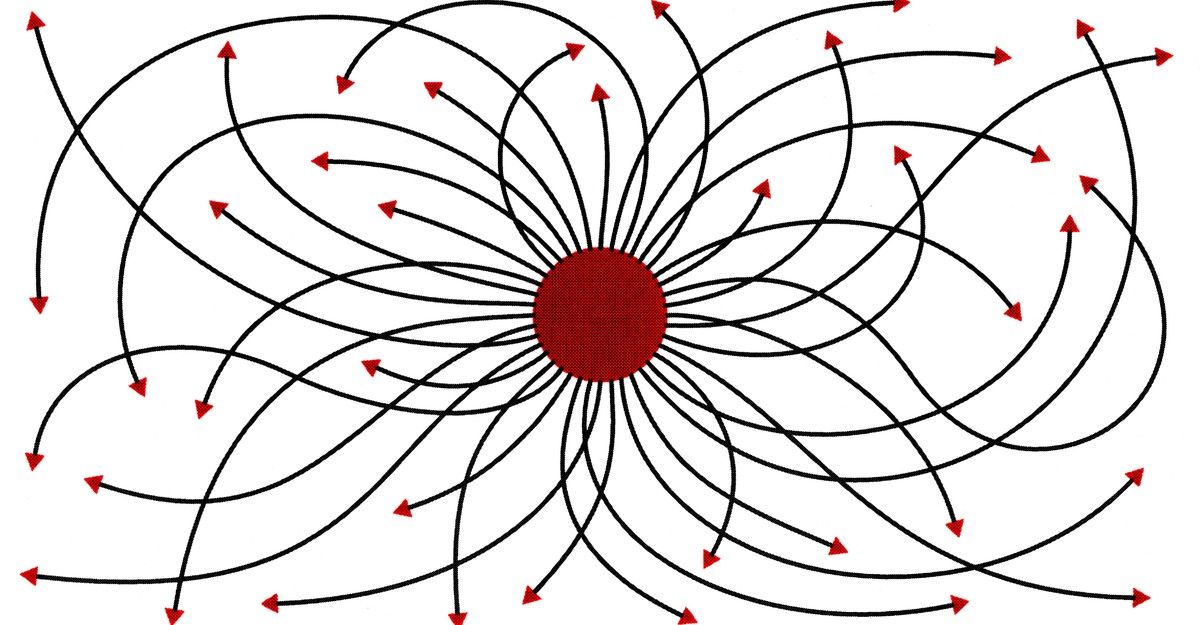
But immune escape isn’t an intrinsic property of any new variant. SARS-CoV-2 is not ascending a ladder with each variant, becoming more and more immune escape-y over time. Rather, think of the coronavirus as an indefatigable rabbit being chased by our immune system, an equally indefatigable dog. The rabbit is always running away from the dog, and the dog is always trying to catch up to the rabbit. The space in which they have to chase each other is so big that it might as well be infinite on human timescales. As Bloom told me previously, the number of possible mutations in SARS-CoV-2 far, far exceeds the number of atoms in the known universe.
Occasionally, the rabbit might make a dramatic Omicron-like leap and shoot out ahead for a while until our immunity catches up. How often this will happen is difficult to predict. “It probably depends on how much of a black-swan event Omicron was,” says Adam Lauring, a virologist at the University of Michigan. Omicron was so different and so unusual compared with everything that had come before. “Could it happen again? Most people think probably not but … you don’t want to be burned twice.” Whether an Omicron-like event happens every two or 20 or 200 years can mean different trajectories for COVID’s future. But at this point, we have only two and a half years of data to go on, so prognosticate at your own risk.
More predictably, though, SARS-CoV-2 is likely to make smaller gains over time, accumulating mutations that make it incrementally better at reinfection. Virologists call this “antigenic evolution.” (Antigenic refers to the parts of a pathogen recognized by our immune system. For SARS-CoV-2, this is predominantly the spike protein.) Different viruses do seem capable of different rates of antigenic evolution. Of the four seasonal coronaviruses that cause common colds, for example, OC43 and 229E are evolving at a rate of 0.3 to 0.5 adaptive mutations in their spike proteins each year. But a third, NL63, doesn’t seem to be changing much at all, says Kathryn Kistler, a virologist also at Fred Hutch who has studied the evolution of the seasonal coronaviruses. She is currently trying to confirm this with blood-serum samples collected in the ’80s and ’90s. And there are so few samples of the fourth coronavirus, HKU1, that we don’t have enough to discern any trend.
Influenza is much better studied, and different types of flu also exhibit different rates of evolution from one another. Of the most common ones, influenza B is the slowest, roughly on par with the coronaviruses OC43 and 229E. H1N1 flu is faster, and H3N2, the predominant flu strain in the world right now, is the fastest. The differences may, at least in part, come down to the shape of the antigen that our immune system recognizes. The spike protein in coronaviruses, for example, needs to change enough so it fools the immune system, but not so much that it stops functioning altogether. H3N2 can get away with a smaller change in its spike-protein analogue: “It’s often one single mutation—sometimes two—[that] can give the virus a huge advantage,” Kistler told me.
Contrast that with measles, a virus that has barely evolved over decades. Our antibodies recognize multiple parts of its key protein. A recent study found that at least five out of eight key sites of that protein need to change at once to erode our immune defenses. A mutation in only one or two of these sites doesn’t confer much of an advantage, but gaining all five at once is very unlikely. So any potential new variants fizzle out, and the dominant measles variant stays quite stable.
SARS-CoV-2, though, has been evolving antigenically faster than any of these viruses, even faster than H3N2. This could come down to the uniqueness of its spike protein, but some of this unusually fast pace over the past two years probably also has to do with the virus being novel. When a new strain of H1N1 “swine flu” hit in 2009, Kistler pointed out, it, too, had an initial burst before slowing down. The coronavirus’s Alpha and Delta variants emerged during a time with many immunologically naive people to infect, and the earliest variants mostly succeeded by becoming more intrinsically transmissible. The virus can only increase its transmissibility by so much, Bloom says, so SARS-CoV-2 is going to have less and less room to improve. However, it can keep finding new ways to get around immunity, as the Omicron subvariants have been doing.
The immunity landscape that SARS-CoV-2 is evolving against is also changing, though. Right now, some people have immunity against the original coronavirus or Alpha or Delta, others have immunity against the Omicron family, and yet others have both. As more variants emerge, our individual exposure history is going to be even more heterogeneous; depending on our previous immunity, some of us might be more susceptible than others to a new variant. The impact will be less uniform. We’ve already seen this with the Omicron subvariants, where countries with smaller previous waves are experiencing bigger BA.5 waves. Some people will also experience more waning immunity than others; older people, for example, tend to mount less durable immune responses to SARS-CoV-2, which is why this group is always prioritized for boosters. Aggressive vaccine updates and booster campaigns would help everyone’s immune system keep up.
Instead of always trying to catch up to the virus though, could we broaden our immunity and get ahead of it? Our current vaccines, while still very good at protecting against severe disease, are not capable of this. The White House is now promoting—though not really funding—next-generation vaccines that could potentially do better: pan-coronavirus vaccines that scientists hope will elicit antibodies against parts of the spike protein that do not change very much, or nasal vaccines to elicit antibodies in the nose and mouth where the virus first replicates, perhaps stopping an infection altogether.
But these ideas are not new to SARS-CoV-2—researchers have been trying these approaches to flu for many years. A universal flu vaccine is still elusive. A nasal flu vaccine, FluMist, does exist, but its effectiveness is quite mixed: It was originally thought to be more effective than the shot, then believed to be less effective—so much so that the CDC pulled the vaccine from 2016 to 2018—until it was reformulated. In any case, it’s clear that FluMist doesn’t come close to preventing all mild flu infections. Barring any major innovations in vaccine technology, our immune systems may be the dog chasing the coronavirus rabbit for a long time still.




















Discussion about this post