Earlier this year we celebrated the 20th birthday of the Office of the Assistant Secretary of Technology Policy/Office of the National Coordinator for Health IT (hereafter ASTP) and reflected on the transformative impact of health IT on patient care delivery in the US. These developments have been instrumental in creating a more connected and patient-focused health care system, supporting our goal of seamless data exchange between health care providers, and enabling real-time access to critical patient health information.
We have authored several blog posts over the past year as part of our series “A Decade of Data Examined” to highlight promising trends and key accomplishments in the areas of interoperability, e-prescribing, public health reporting, and patient access to health information. The trends examined across these blog posts show striking changes across the health care system’s landscape in a relatively short time:
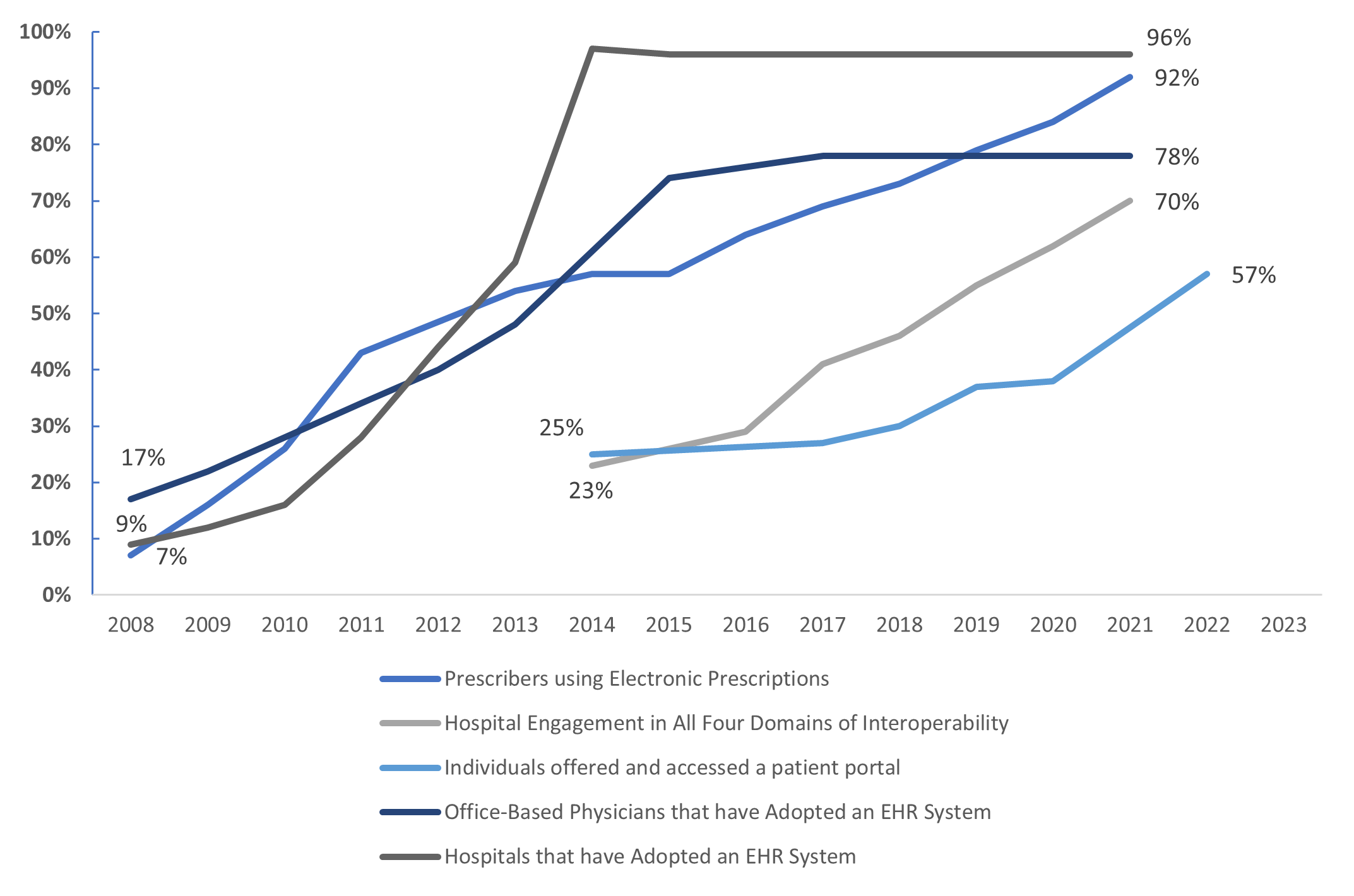
- Rates of interoperability have increased; 70% of hospitals now engage in all four domains of electronic data exchange: electronically finding, sending, receiving, and integrating patient health information, up from just 23% in 2014. This has enhanced care coordination and patient outcomes and is helping to support seamless information sharing across health care systems. Still, persistent challenges in data integration and standardization demonstrate the need to address persistent barriers to exchange and continue efforts to promote interoperability nationwide.
- Over the past decade, e-prescribing has become nearly universal, with 92% of prescribers now using e-prescribing systems. This shift has helped improve prescription accuracy and patient safety, especially through the increased use of electronic prescribing for controlled substances. Challenges remain in achieving consistent adoption across all health care settings, emphasizing the need for continued efforts to optimize e-prescribing practices, particularly regarding prior authorization processes.
- The last decade has seen significant advancements in public health reporting; 90% of hospitals now electronically report immunization data, up from 63% in 2012. Data show marked improvement in hospitals’ ability to electronically report immunizations, laboratory results, and syndromic surveillance data, all of which are important for timely and effective public health response, especially during emerging health threats.
- Patient access to electronic health information has also improved; 97% of hospitals and 65% of physicians now offer online access to health records. This expansion has empowered patients to more actively engage in their health care, with patient access to their online medical record more than doubling from 25% in 2014 to 57% in 2022. However, disparities in access and usage persist, underscoring the need for targeted efforts to ensure all patients have equitable opportunities to access their health information electronically.
Our recently published manuscript, The Evolution of Health Information Technology for Enhanced Patient-Centric Care in the United States, takes a deep dive into these advancements through data-driven analyses, and offers insights and recommendations for the road ahead. The paper explores how health IT has evolved from a supplementary tool to a central component of patient care. We detail the progress made by examining key advancements, legislation, and initiatives. We also highlight ongoing challenges, especially in achieving nationwide interoperability and addressing equity issues. Lastly, we offer insights and recommendations for the future of health IT to enhance patient-centric care.
Growth of Health IT for Enhanced Patient-Centric Care
We are excited about the future of health IT and its potential to transform patient care over the next decade. Newer initiatives like TEFCA and proposed rulemaking in HTI-2 have set the stage for even more advancements in how health information is shared, accessed, and used and help mitigate identified barriers to bi-directional exchange. Integrating advanced technologies, such as artificial intelligence (AI) and machine learning, within health IT systems promises to support more personalized, efficient, and accessible health care. ASTP now leads the coordination of AI policy across HHS and engages in public-private initiatives to actively shape the AI landscape. This will help to ensure AI’s use in health and human services is fair, appropriate, valid, effective, and safe. We are optimistic about these technological innovations and look forward to continued collaboration, improving patients’ access to their health information, and health care providers leveraging a growing number of cutting-edge tools to deliver high quality care.
Acknowledgment: The Decade of Data Examined blog series and The Evolution of Health Information Technology for Enhanced Patient-Centric Care in the United States paper were authored by ASTP staff, including Wesley Barker, Wei Chang, Jordan Everson, Meghan Gabriel, Vaishali Patel, Chelsea Richwine, and Catherine Strawley.




















Discussion about this post