A team of US researchers has developed an AI algorithm that can spot clinically significant prostate cancer on MRI scans.
The researchers say that the deep learning model could help radiologists to detect the cancer.
They’ve published their findings in Radiology.
Prostate cancer is one of the most common cancers in the world, with the World Health Organization recording 1.41 million new cases of the disease in 2020.
Spotted early, it is easy to treat. With early detection and treatment, more than 98% of people diagnosed with prostate cancer will survive for more than 5 years after diagnosis.
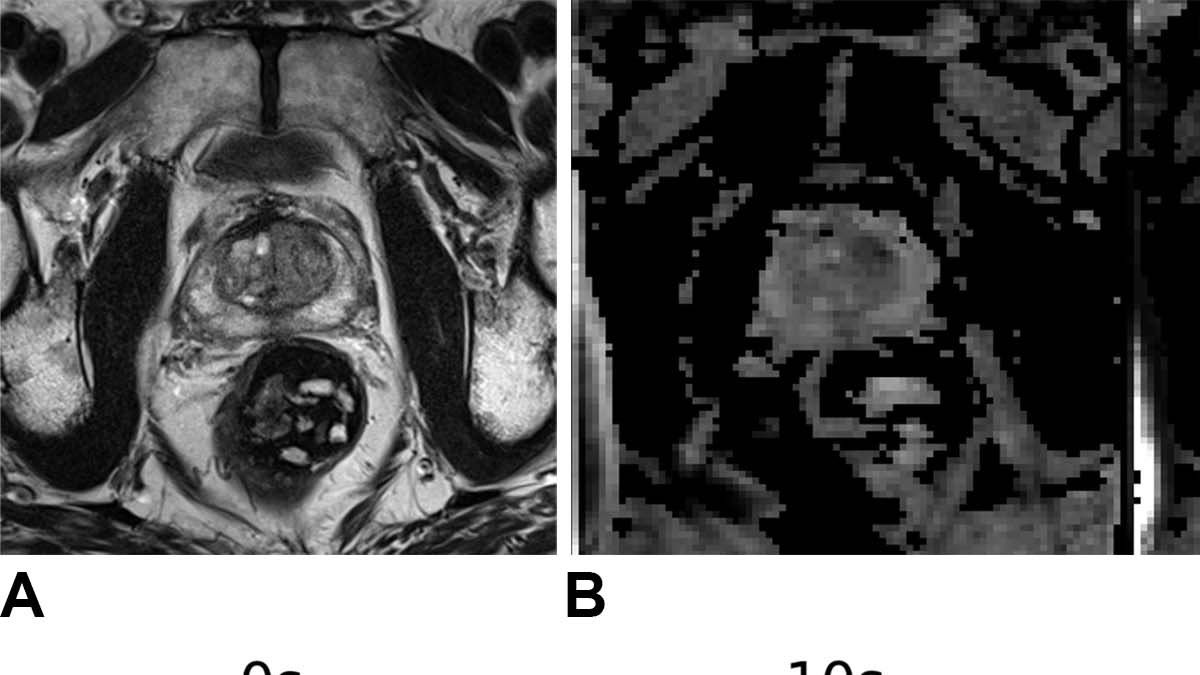
Usually, prostate cancer is detected by radiologists through a series of MRI sequences.
“The interpretation of prostate MRI is difficult,” says senior author Dr Naoki Takahashi, from the Department of Radiology at the Mayo Clinic, USA.
“More experienced radiologists tend to have higher diagnostic performance.”
Researchers have previously sought to train machine learning programs with MRI imagery to spot prostate cancer. But they typically need annotated MRI scans – that is, scans with diagnostic notes added by radiologists or pathologists to specific lesions which may be cancerous.
“Radiologists annotate suspicious lesions at the time of interpretation, but these annotations are not routinely available, so when researchers develop a deep learning model, they have to redraw the outlines,” says Takahashi.
“Additionally, researchers have to correlate imaging findings with the pathology report when preparing the dataset. If multiple lesions are present, it may not always be feasible to correlate lesions on MRI to their corresponding pathology results. Also, this is a time-consuming process.”
These researchers used a different approach, by training a convolutional neural network – a type of AI designed to be good at analysing images – to examine scans without needing specific information about where the lesion is.
Then, they tested their AI out on data from prostate examinations. They found that the algorithm worked as well as experienced radiologists at detecting prostate cancer, but the combination of the algorithm and radiologists’ findings performed better than both individually.
“I do not think we can use this model as a standalone diagnostic tool,” says Takahashi.
“Instead, the model’s prediction can be used as an adjunct in our decision-making process.”
The researchers are now using more data to train the model, and are planning to see how radiologists interact with it.
“We’d like to present the model’s output to radiologists and assess how they use it for interpretation and compare the combined performance of radiologist and model to the radiologist alone in predicting clinically significant prostate cancer,” says Takahashi.


















Discussion about this post