A drug commonly used for managing Alzheimer’s symptoms has the potential to put the body on ‘pause’ in emergencies where every second counts.
A team led by researchers from the Wyss Institute for Biologically Inspired Engineering, a part of Harvard University, tested the drug donepezil hydrochloride (DNP) on tadpoles, which put them into a state of dormancy known as torpor.
In nature, a variety of animals go into torpor for days or weeks, experiencing significant drops in body temperature and metabolism to preserve energy. Similar to seasonal hibernation, torpor’s brief periods of rest typically occur during periods of low food availability.
Being able to induce a torpor-like state in humans has benefits in medical settings where it may bide doctors more time to save their patient. The team behind this research thinks DNP – already FDA approved for use in humans – could help prevent permanent organ damage that sometimes occurs while a person is being transported to hospital.
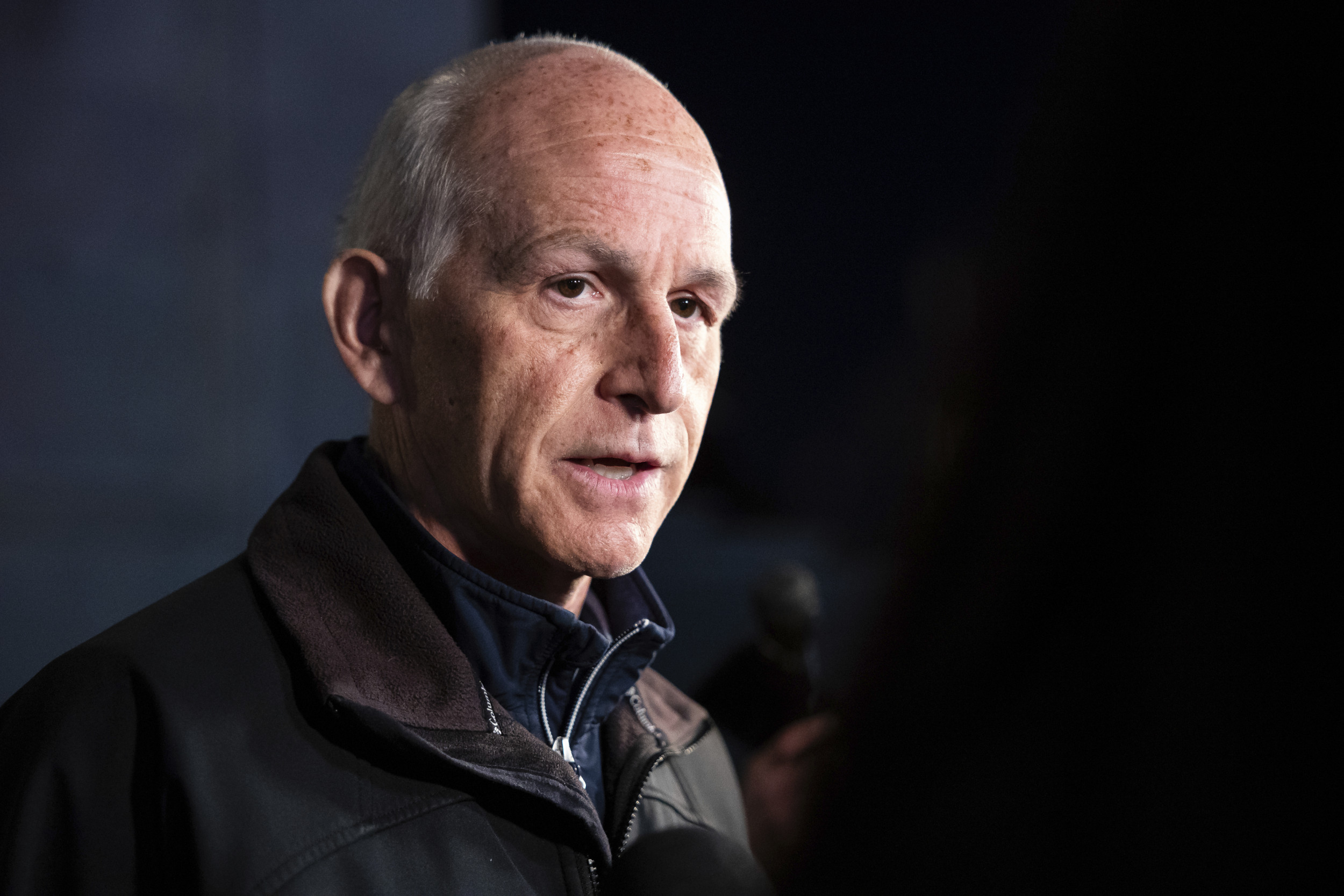
“Cooling a patient’s body down to slow its metabolic processes has long been used in medical settings to reduce injuries and long-term problems from severe conditions, but it can only currently be done in a well-resourced hospital,” says immunologist Michael Super from Harvard University.
“Achieving a similar state of ‘biostasis’ with an easily administered drug like DNP could potentially save millions of lives every year.”
It’s important that an organism going into torpor comes back out of the state safely. In a previous study, the researchers found that a different drug, SNC80, also induced torpor in tadpoles of the African clawed frog (Xenopus laevis).
These creatures don’t naturally hibernate or experience torpor, so the scientists knew the drug had been successful when all the tadpoles’ swimming slowed down, suggesting their metabolisms were suppressed by the drug. Unfortunately the compound isn’t a viable option for use in humans due to its tendency to cause seizures.
To find a safer candidate, the research team used a machine learning-based computational algorithm called Network Models for Causally Aware Discovery (NeMoCAD) to sift out 378 compounds likely to trigger similar reactions to SNC80 in the frogs.
Out of all of the possibilities, DNP bore the closest structural similarities. In some ways, it comes as little surprise – overdoses in Alzheimer’s patients has been reported to coincide with slowed heart rate and lethargy.
“However, while free DNP drugs can suppress metabolic activity in tadpoles, their use was limited by their toxicity, which appeared after administration for more than 2−3 hours,” the team writes. The torpor state in these initial tests that lasted for longer than four hours was irreversible
Noticing the drug was accumulating in all tissues throughout the tadpole’s body, the team overcame the issue by trapping it inside a nano-emulsion. Essentially a tiny capsule with one liquid as the cap and another as the contents, this “significantly reduced its toxicity while maintaining its efficacy,” delivering a higher concentration of DNP to the brain, but with a slower, more controlled release to the rest of the body.
And that meant the tadpoles could be kept in torpor for longer, temporarily reducing their mobility, heart rate, and oxygen consumption. All “fully reversible”, according to the study.
“Additional advantages of this approach include DNP’s previous approval for clinical use by the FDA, low toxicity of the nano-emulsions, manufacturing scalability, and the possibility to administer treatments without the need for trained personnel (eg using noninvasive mucosal routes),” the authors write.
It’s still a long road before DNP is being used in the back of an ambulance to buy precious time, but it’s exciting to think that existing drugs could be repurposed in ways we haven’t even thought of yet.
This research was published in the American Chemical Society’s ACS Nano.



















Discussion about this post