For decades, scientists have been puzzled by a mysterious type of antibiotic resistance. Called “heteroresistance,” it occurs when a tiny fraction of bacteria in a population can evade antibiotics, and it is almost impossible to detect with routine clinical tests. Yet some scientists think heteroresistance could be the culprit behind many antibiotic treatment failures.
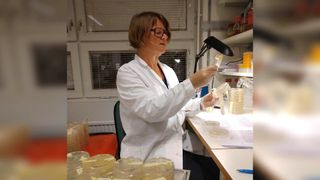
Karin Hjort, a microbiologist at Uppsala University in Sweden, is a leading expert on heteroresistance. Live Science spoke with Hjort about what heteroresistance is and what implications it has for the fight against superbugs.
(This interview has been edited for clarity and length.)
Kristel Tjandra: Can you tell me what heteroresistance is?
Karin Hjort: The definition of heteroresistance is that you have, within a mainly antibiotic-susceptible population, a subpopulation that is resistant. This subpopulation should be of a certain size. In most cases, it is 10^-7 [one ten-millionth] colony-forming unit, or viable bacterial cell, per milliliter of broth. The resistance level should also be of a certain times higher — usually eightfold — than the main population.
KT: Is heteroresistance a new phenomenon? How is this different from antibiotic resistance in a general sense?
KH: It’s nothing new. Think of it as a type of antibiotic resistance. All the studies we have done so far pointed in the same direction: that heteroresistant populations become resistant in the same way that a full population could become resistant. But the difference here is that this tiny subpopulation can survive higher concentrations of antibiotics than the rest of the population. If you put an antibiotic — selection pressure — that resistant subpopulation will quickly outgrow the others. And when you take away their selection pressure, the few [susceptible cells] that survived without becoming resistant will eventually outcompete the resistant ones.
KT: So, in other words, the population can switch between resistant and susceptible very rapidly?
KH: In a sense, yes.
KT: We tend to speak of antibiotic-resistant and antibiotic-susceptible bacteria as black-and-white categories. Is it possible that heteroresistance is this gray area, a midpoint where the bacteria go from being susceptible to becoming resistant?
KH: Yes, definitely. It could be a way of going from being susceptible to resistant. [But] they don’t become resistant unless you treat them with antibiotics. When that happens, the resistant subpopulation survives, whereas the main population that is susceptible dies off the treatment. So, in that sense, you can say that heteroresistance is a step towards resistance. But the isolate will still be heteroresistant the next time we test them.
Related: Dangerous ‘superbugs’ are a growing threat, and antibiotics can’t stop their rise. What can?
KT: What do these tests look like?
KH: In a research lab, we do a population analysis profile to test if an isolate is heteroresistant. (Editor’s note: Population analysis profiling involves testing bacteria at different population densities with different concentrations of antibiotics to see what proportion of the population is resistant to the drug.) But you cannot do this analysis in a clinical lab because it is time-consuming and very labor-intensive.
KT: From your study, how might bacteria develop heteroresistance?
KH: Some are resistant because they gain mutations. But instead of everyone in the population being resistant, it’s only a portion of the population that is resistant. There are others that we consider unstable and acquire their resistance through amplifications of genes, which means that they have higher gene expression that leads to resistant phenotype.
KT: Can all types of bacteria become heteroresistant?
KH: I think all bacteria have the ability to become heteroresistant, but the mechanisms can vary.
KT: Can all antibiotics trigger heteroresistance?
KH: I’m not sure if all antibiotics actually will lead to heteroresistance since we haven’t done large enough studies to show that. I think it depends on which antibiotics and bacteria.
KT: Is heteroresistance something to be worried about in the clinical setting?
KH: Heteroresistance towards some antibiotics seems to be common in clinical isolates. And maybe that’s why treatment fails. Failure could mean that the patient dies, which I don’t think is that common because usually, you change to another antibiotic. But failure could also mean that the patient has to stay in the hospital longer, and that is problematic.
KT: What do you hope to see in the future with a better understanding of heteroresistance?
KH: For me, I would like to see in front of me a list that tells me whether a strain is heteroresistant towards an antibiotic. And if it’s heteroresistant, then don’t treat them with that antibiotic. Basically, it’s the kind of clinical answer for the clinicians to make a treatment decision. Also, [I hope there will be a way] to find a way to test these heteroresistant strains in the hospital.
We are working on some techniques now to try to figure out better ways of testing these [heteroresistant] bacteria. You need to have something easier and faster [than population analysis profiling].



















Discussion about this post