New
Zealand’s second Omicron wave might just be easing up,
with the latest data showing we seem to be in a downward
trend. So are those who never got Covid-19 now in the
minority?
The SMC asked experts about what the latest
data say about rates of infection, what we still don’t
know, and how this affects wider immunity to the
virus.
Professor Michael Plank, Te Pūnaha Matatini
and University of Canterbury, comments:
What do the
data tell you about how many New Zealanders have or
haven’t been infected?
“The true number of people
who’ve had Covid-19 is unknown because we only know about
cases who get tested and report their result. The proportion
of infections that are reported is probably somewhere
between 40% and 65%. It’s unlikely to be much less than
40% because at least 40% of all 20-25 year olds have already
reported a case. On the other hand the reported infection
rate is typically less than 65% of the infection rate in
routinely tested cohorts such as border workers. This means
it’s likely that at least half of New Zealanders have had
Covid-19, although those that haven’t probably still
represent a significant minority.”
What does this
mean for our herd immunity to Covid?
“The lack of
an accurate estimate for the true number of infections
creates uncertainty about how much immunity there currently
is in the population. This makes it harder to estimate the
potential size of future waves of Covid-19 or the impact of
new variants. The best way to get an accurate picture of the
true number of infections would be to systematically test a
representative sample of the population on a regular basis.
This would provide high-quality ongoing data about the level
of Covid-19 in the community and reduce our reliance on
self-reported test results.”
Conflict of interest
statement: “Michael Plank is funded by the Department of
Prime Minister and Cabinet for mathematical modelling of
Covid-19.”
Professor Mike Bunce, Principal
Scientist (Genomics), Institute of Environmental Science and
Research, comments:
What do the data tell you about
how many New Zealanders have or haven’t been
infected?
“Last week the official tally of
registered cases in Aotearoa New Zealand was approximately
1.62 million people. We know that this number is under the
true number of infections due to asymptomatic cases,
non-reporting of positive cases, reinfections and
failure/unwillingness to test (even if unwell). The Ministry
of Health is planning a prevalence survey that will be key
in ascertaining the true number of infections, as a
person’s antibody profile can tell us if a person has been
previously exposed to the virus (as opposed to the vaccine).
In the UK, this approach showed that >95% of the
population has been exposed to SARS-CoV-2 in the pandemic,
many of these are recent infections. Looking at one cohort,
primary school students, in November 2021 approximately 40%
(pre Omicron) of students had been exposed. In March of 2022
this number was >80%.
“What we do know from our
genomic surveillance here in Aotearoa is the approximate
proportions of each of the variants (see figure and embedded
table). This temporal infection history is important as the
variants of SARS-CoV-2 that we are exposed to (coupled with
vaccines and time since infection) are key factor in
determining the traction new forms of SARS-CoV-2 will have.
For example, the reason that the BA.5 wave here in New
Zealand was at the lower end of the modelling predictions
could be because our population was heavily exposed to the
BA.2 variant of Omicron which is closer to BA.5 than
original BA.1.
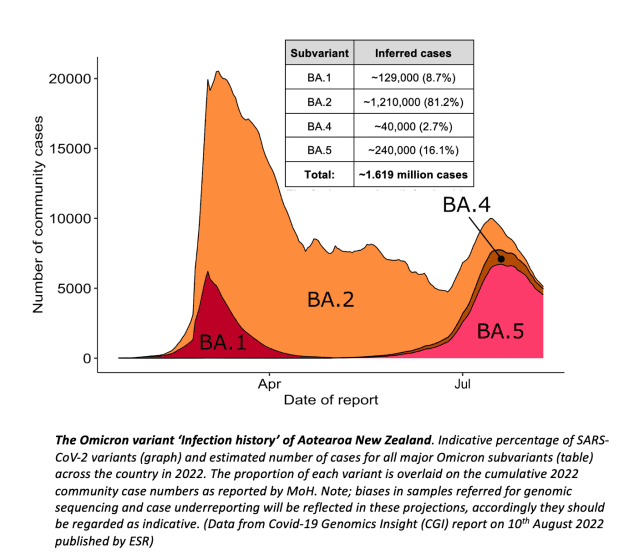
credit: ESR
What do we still
not know? What data do we still need?
“The serology
survey (soon to be conducted) and modelling of this data in
concert with hospitalisation rates and wastewater will
likely provide a more nuanced picture of the total number of
Kiwis that have been exposed to Covid-19 – but working out
the ‘true’ number of infected (and reinfected) people
will always remain a challenge. High rates of participation
in initiatives like FluTracker may also facilitate better
estimates of symptomatic infections across the Motu. There
are aspirations here at ESR to better characterise the
(often seasonal) viruses that sweep Aotearoa using the
genomic toolkit that we have developed during the pandemic.
For example, PCR testing (or genomics) that can distinguish
RSV, flu, Covid-19 or other viruses that give us ‘colds’
can be used to better understand the exact virus that is
driving illness, and what strain of each virus is
present.
What does this mean for our herd immunity to
Covid?
“Determining how susceptible/resilient a
population is to new wave of Covid-19 is a complex interplay
of; (i) vaccine and booster rates (ii) percentage of the
population with protective immunity (iii) time since
infection/vaccines (iv) new variants of SARS-CoV-2 that
might escape prior immunity (v) Mask use and other social
factors such as staying at home while sick (vi) the efficacy
of pharmaceuticals to treat Covid-19 patients and reduce
viral loads and, (vii) the development of new vaccines that
might reduce/prevent infections.
“Taken together,
this shopping list of factors paints a picture of why it is
difficult to predict how protected or vulnerable New
Zealanders might be. While we would like to be more certain
what the virus’s next move might be, history has taught us
that diseases are adept at changing the ‘playing field’
and as we adapt our strategies we nudge the virus in
different directions. So while we may well estimate a level
of ‘herd immunity’ that might be protective one week, it
may change the next. Predicting the trajectory of ‘new’
RNA viruses such as SARS-CoV-2 adds another layer of
difficulty as they continue to rapidly explore different
ways to gain a fitness advantage in a new
host.”
Conflict of interest statement: “ESR
receives funding from the Ministry of Health to process
clinical samples for whole genome sequencing and
wastewater.”
Dr Dion O’Neale, Project Lead,
COVID Modelling Aotearoa; and Senior Lecturer, Physics
Department, University of Auckland, comments:
What do
the data tell you about how many New Zealanders have or
haven’t been infected?
“Data from the Ministry of
Health records just under 1.7 million confirmed cases of
COVID-19 in Aotearoa New Zealand. Of these, just over 28,000
cases are recorded as probable reinfections in people who
have been a confirmed case of COVID-19 twice or more. Both
the number of confirmed cases and the number of recorded
reinfections will be a significant under-estimate of the
true number of infections. This is because not all
infections end up being recorded as a case.
“The
ratio of the number of infections in the community to the
number of confirmed cases that we know about is called the
case ascertainment rate, or CAR. This rate will typically
change over time, depending on a number of factors such as
how easy it is for people to access tests and how inclined
they are to seek a test and to report the result. Most
estimates of the CAR put it above 33% but probably below
50%. If we ignore reinfections this means that the number of
infections that we have had in Aotearoa is (at least)
roughly twice the number of confirmed cases — so over 3
million.
“The effect of the case ascertainment rate
on estimates of the number of reinfections is a little more
complicated. This is because the CAR applies for both the
first infection and for later infections. If someone’s
infection was not recorded as a confirmed case the first
time around then – even if their second infection was
recorded as a confirmed case – it will not be captured as
a reinfection and we will be underestimating the number of
reinfections, or possibly overestimating the number of
unique people who have been infected. This can matter for
disease modelling as the immunity history (the combination
of past vaccinations and infections) of people affects what
the landscape looks like for how susceptible the population
might be for future infections, including with any new
variants.
“Under-reporting of infections can happen
for a number of different reasons; some people may have
confirmed their infection with a rapid antigen test, but not
reported the result; some people may have been symptomatic
and not wanted to use a RAT to confirm their infection, or
may have had a false negative on their RAT due to test
timing or technique; and a sizable number of people may have
not even had symptoms to alert them that they might need to
test for an infection. Estimates are that as many as 40% of
infections may be asymptomatic. Unless these people know
that they have been in contact with a confirmed case – for
example, a family member who has tested positive – or
unless they are testing independently of symptoms, these
people may never have had a reason to test during their
infection.
“Methods like wastewater sampling (e.g.
see the ESR
dashboard) can help us to better understand patterns in
infections and cases, based on how much RNA from SARS-CoV-2
is detected in wastewater, but such methods can be tricky to
calibrate. And while wastewater methods can be useful for
indicating when the case ascertainment rate in a region
might be changing (i.e., if the amount of detected
SARS-CoV-2 RNA is going up but the number of confirmed cases
is not, then case ascertainment is probably getting worse),
it is more difficult for it to tell us what the estimated
number of total infections behind that signal might
be.
“One of the best ways to get a good estimate of
the true number of infections in the community is through
what is called an infection prevalence survey. This includes
methods like that taken by the ONS
in the UK. An infection prevalence survey uses regular
samples from sub-set of the population to calculate the
prevalence of COVID-19 in the community over time and
accounting for differences in location and
population.
“In Aotearoa, the Ministry of Health
announced in July that they would be starting such and
infection prevalence survey. Once underway, this will give
extremely useful information about infections in the
community and how they are distributed. Infection prevalence
surveys give an indication of current infections. They are
often combined with something called a sero-prevalence
survey. Rather than looking for indication of RNA or protein
from a current COVID-19 infection, sero-prevalence surveys
look for the presence of COVID-19 antibodies from past
infection. While antibody markers do fade over time,
seroprevalence surveys can help to give us a view back to
past infections, even when people have now
recovered.
“Information from this sort of survey is
useful in figuring out how much protection from past
infection communities are likely to have and what the
susceptibility landscape looks like for the population in
Aotearoa.”
Conflict of interest statement: “I,
along with others from COVID Modelling Aotearoa, am funded
by the Department of Prime Minister and Cabinet to provide
advice on the COVID response and from a Health Research
Council grant to look at equity related to COVID in
Aotearoa.”
© Scoop Media




















Discussion about this post