Researchers have created a prototype for what they call “living bioelectronics”: a combination of living cells, gel, and electronics that can integrate with living tissue.
For years, Bozhi Tian’s lab has been learning how to integrate the world of electronics—rigid, metallic, bulky—with the world of the body—soft, flexible, delicate.
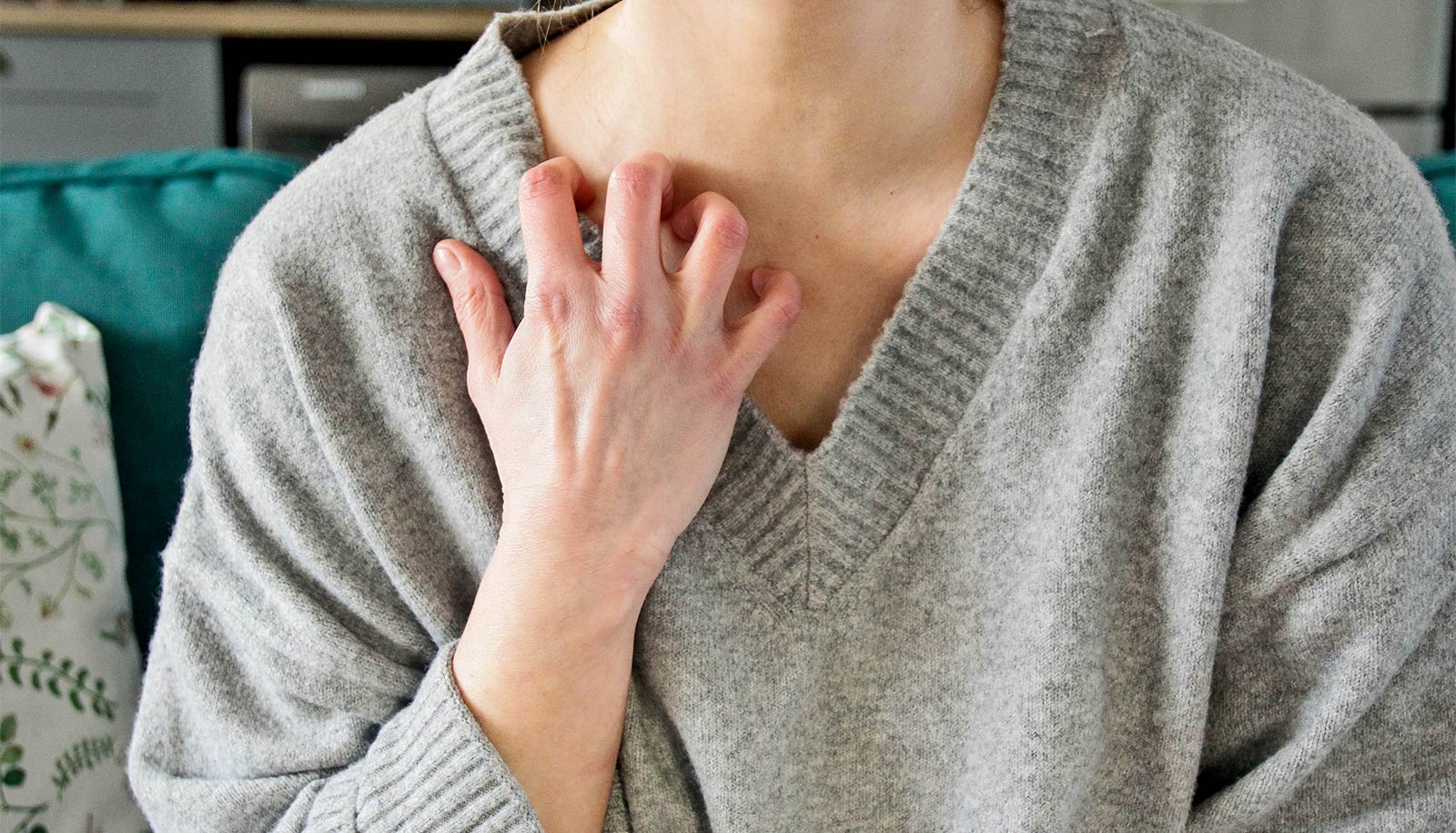
The new patches are made of sensors, bacterial cells, and a gel made from starch and gelatin. Tests in mice found that the devices could continuously monitor and improve psoriasis-like symptoms, without irritating skin.
“This is a bridge from traditional bioelectronics, which incorporates living cells as part of the therapy,” says Jiuyun Shi, the co-first author of the paper and a former PhD student in Tian’s lab (now with Stanford University).
“We’re very excited because it’s been a decade and a half in the making,” says Tian.
The researchers hope the principles can also be applied to other parts of the body, such as cardiological or neural stimulation.
Pairing electronics with the human body has always been difficult. Though devices like pacemakers have improved countless lives, they have their drawbacks; electronics tend to be bulky and rigid, and can cause irritation.
But Tian’s lab specializes in uncovering the fundamental principles behind how living cells and tissue interact with synthetic materials; their previous work has included a tiny pacemaker that can be controlled with light and strong but flexible materials that could form the basis of bone implants.
In this study, they took a new approach. Typically, bioelectronics consist of the electronics themselves, plus a soft layer to make them less irritating to the body.
But Tian’s group wondered if they could add new capabilities by integrating a third component: living cells themselves. The group was intrigued with the healing properties of certain bacteria such as S. epidermidis, a microbe that naturally lives on human skin and has been shown to reduce inflammation.
They created a device with three components. The framework is a thin, flexible electronic circuit with sensors. It is overlaid with a gel created from tapioca starch and gelatin, which is ultrasoft and mimics the makeup of tissue itself. Lastly, S. epidermidis microbes are tucked into the gel.
When the device is placed on skin, the bacteria secrete compounds that reduce inflammation, and the sensor monitors the skin for signals like skin temperature and humidity.
In tests with mice prone to psoriasis-like skin conditions, there was a significant reduction in symptoms.
Their initial tests ran for a week, but the researchers hope the system—which they term the ABLE platform, for Active Biointegrated Living Electronics—could be used for a half-year or more. To make the treatment more convenient, they say, the device can be freeze-dried for storage and easily rehydrated when needed.
Since the healing effects are provided by microbes, “It’s like a living drug—you don’t have to refill it,” says Saehyun Kim, the other co-first author of the paper and a current PhD student in Tian’s lab.
In addition to treating psoriasis, the scientists can envision applications such as patches to speed wound healing on patients with diabetes.
They also hope to extend the approach to other tissue types and cell types. “For example, could you create an insulin-producing device, or a device that interfaces with neurons?” says Tian. “There are many potential applications.”
Tian says this is a goal he has harbored since his time as a postdoctoral researcher nearly 15 years ago, when he first began experimenting with “cyborg tissues.”
“Since then, we’ve learned so much about the fundamental questions, such as how cells interface with materials and the chemistry and physics of hydrogels, which allows us to make this leap,” he says. “To see it become reality has been wonderful.”
“My passion has always been to push the boundaries of what is possible in science,” says Shi. “I hope our work could inspire the next generation of electronic designs.”
The study appears in Science.
Additional authors are from the University of Chicago, Rutgers University, and Columbia University.
The researchers used the Soft Matter Characterization Facility and the Pritzker Nanofabrication Facility at the University of Chicago. They are also working with the Polsky Center for Entrepreneurship and Innovation to commercialize the technology.
Funding for the work came from the US Army Research Office, the National Science Foundation, the Chan Zuckerberg Biohub Acceleration Program, a University of Chicago startup grant, and a Rutgers University startup grant.
Source: University of Chicago


















Discussion about this post