An Oakland County resident is the first in Michigan to have a probable case of the monkeypox virus, state health officials said Wednesday.
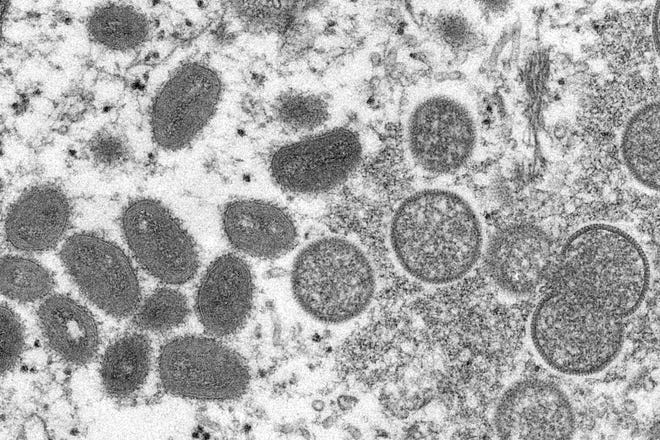
The virus, which is in the orthopoxvirus family and is closely related to smallpox, is part of a global outbreak of more than 5,115 cases that now have spread to at least 27 states, the District of Columbia and 51 countries outside of its endemic areas as of June 29, according to the U.S. Centers for Disease Control and Prevention.
Preliminary testing by the state Bureau of Laboratories showed a presumptive positive result for orthopoxvirus. Testing to confirm that is now underway by the CDC.

More:‘Rare and unusual’ monkeypox cases are causing global concern. Here’s what we know.
More:First US case of monkeypox this year found in Massachusetts, confirmed by CDC
The person is isolating and does not pose a risk to the public, state health officials said in a statement.
“Monkeypox is a viral illness that spreads primarily through direct contact with the infectious rash, scabs, bodily fluids or prolonged face-to-face contact,” said Dr. Natasha Bagdasarian, the state’s chief medical executive. “It is important to remember that the risk to the general public is low. However, Michiganders with concerns about monkeypox should see their provider to be evaluated for testing.”
No other details were released Wednesday about the Oakland County resident.
More national attention and resources are being devoted to the outbreak as the number of confirmed monkeypox cases in the U.S. has more than doubled within a week’s time — rising from 156 on June 22 to 351 on Wednesday, according to the CDC.
The agency launched its Emergency Operations Center on Tuesday to respond to the outbreak, dedicating more than 300 employees to coordinating the emergency response and increasing vaccine distribution and testing.
The first U.S. case was identified in a man from Massachusetts, who was admitted May 12 to Massachusetts General Hospital in Boston. The man hadn’t been in contact with animals known to carry monkeypox and didn’t travel to central or western Africa, where the virus ordinarily is found.
Since then, 350 more cases were confirmed as of Wednesday in Arizona, California, Colorado, the District of Columbia, Florida, Georgia, Hawaii, Illinois, Indiana, Kentucky, Maryland, Massachusetts, Minnesota, Missouri, Nebraska, Nevada, New Jersey, New York, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, Texas, Utah, Virginia and Washington, according to the CDC and state health officials.
What is monkeypox?
Monkeypox was first identified in 1958 in monkeys in the Democratic Republic of Congo. It wasn’t until 12 years later, in 1970, that the first human cases were identified. Infected rodents and squirrels and nonhuman primates can be carriers of the virus.
It causes less severe disease than smallpox, but monkeypox infections still are serious.
There are two known types. The West African clade is estimated to be fatal in 1 in 100 people, but an infection with the Congo Basin clade is deadlier. Its mortality rate is about 1 in 10, according to the World Health Organization.
“The strain and the identified cases, both in the United States and globally, is West African strain which is the milder of the two strains of monkeypox virus,” said Dr. Jennifer McQuiston, deputy director of the Division of High Consequence Pathogens and Pathology at the CDC, who is leading the investigation of the outbreak. “Most people who are infected with monkeypox recover within two to four weeks without specific treatments.”
No deaths have been reported among any of the cases so far, she said, and the risk to the general public remains low.
More:US to release at least 1.6 million vaccines to fight monkeypox by end of year, officials say
“That being said, we don’t want to minimize this condition,” McQuiston said. “The rash caused by monkeypox virus can spread widely across the body or present in sensitive areas like the genitalia. It can be really painful and some patients have reported needing prescription pain medicine to manage that pain. The sores can also cause long-term scarring on the skin.”
Even mild rashes with only one lesion should be investigated, McQuiston said.
“I want to emphasize that this could be happening in other parts of the United States. There could be community level transmission that is happening and that’s why we want to really increase our surveillance efforts,” she said.
“We want to really encourage physicians that if they see a rash and they’re concerned it might be monkeypox to go ahead and test for that.”
Why are cases in the U.S. and Europe so unusual?
Monkeypox cases have been reported in the tropical rainforest areas of western and central Africa. Infections in people outside of Africa aren’t common and have been linked to international travel or imported animals.
Health officials are trying to understand why the virus is spreading so quickly and so far afield now and they’re trying to determine whether the infections in Europe, Canada and the U.S. are related.
Genetic sequencing of the virus that infected the man from Massachusetts who had the first known U.S. case closely matches the sequencing from a patient with monkeypox in Portugal, McQuiston said.
“We immediately shared this information publicly … so that the rest of the world can compare it to their sequence data,” she said. “We feel like this kind of public sharing of early sequence data is going to be important for all countries to do so that we can all better understand how the virus is spreading across the globe.”
It has many concerned because it is the first time that such transmission has been reported without known epidemiological links to west and central Africa, according to the European Centre for Disease Prevention and Control.
More:How a global shortage of contrast dye is affecting CT scans, tests at Michigan hospitals
More:Many metro Detroit stores have limited supplies of baby formula, limiting purchases
Some of the cases, but not all, include those who self-identify as men who have sex with men, the CDC reported.
“Many of these global reports of monkeypox cases are occurring within sexual networks,” said Dr. Inger Damon, a poxvirus expert who is director of the CDC’s division of high-consequence pathogens and pathology. “However, health care providers should be alert to any rash that has features typical of monkeypox.
“We’re asking the public to contact their health care provider if they have a new rash and are concerned about monkeypox.”
What are the symptoms?
It can take up to 21 days for symptoms to develop after a person is infected, according to the CDC. But when symptoms appear, they are typically flu-like and include the swelling of lymph nodes. Common are:
- Fever
- Headache
- Muscle aches
- Backache
- Swollen lymph nodes
- Chills
- Exhaustion
From one to three days after the flu-like symptoms begin, people typically develop a rash and lesions that may start in one place on the body and spread to other parts.
Lesions progress through stages and scab before falling off.
The illness typically lasts two to four weeks, and could initially be confused with a sexually transmitted disease such as syphilis or herpes.
More:2 Michigan kids suspected of having rare form of severe hepatitis under CDC investigation
More:16 Michigan counties now at high level of COVID-19 transmission. CDC says wear a mask.
How does monkeypox spread?
The virus can spread from person to person if there’s contact with body fluids, monkeypox sores or contaminated clothing and bedding, according to the CDC. In that way, monkeypox enters the body through broken skin, the respiratory tract or the eyes, nose or mouth.
It also can be transmitted through respiratory droplets from prolonged exposure to an infected person who is coughing or sneezing. During pregnancy, the virus also can cross the placenta from mother to fetus.
The CDC recommends using personal protective equipment such as masks and gloves when caring for people with monkeypox as the virus may spread through respiratory secretions when people have close, face-to-face contact.
In parts of central and western Africa, people can be exposed to monkeypox through bites or scratches from rodents and small mammals that are infected, when preparing wild game, or having contact with an infected animal or possibly animal products.
“People can become infected with monkeypox through close, sustained skin-to-skin contact with someone who has an active rash or through respiratory droplets in someone who has lesions in their mouth and they’re around another person for an extended period of time,” McQuiston said.
“What we’re talking about here is close contact. It’s not a situation where if you’re passing someone in the grocery store, they’re going to be at risk for monkeypox.”

Those at highest risk would be family members of an infected person or health care workers who treat someone with an infection, McQuiston said.
The CDC recommends isolation for people with known cases of the virus and tracing close contacts.
“We’ve seen over the years that often the best way to deal with cases is to keep those who are sick, isolated so that they can’t spread the virus to close family members and loved ones and to follow up proactively with those that a patient had contact with so that they can watch for symptoms,” McQuiston said.
Of U.S. cases as of June 3, she said: “All patients are in recovery or have already recovered, and those who still have a rash are being advised to stay home and stay away from other people until they’re fully recovered. That means when all of the sores have scabbed over the scabs fall off and new healthy skin has emerged.”
Is monkeypox only spreading among gay and bisexual men?
Some, but not all cases identified so far are among gay and bisexual men. However, anyone can develop and spread a monkeypox infection, said Dr. John Brooks, a medical epidemiologist in the CDC’s Division of HIV/AIDS Prevention.
“By no means is the current risk of exposure to monkeypox exclusively to the gay and bisexual community in the U.S.,” he said during a late May news conference. However, “many of those affected in the current global outbreak identify as gay and bisexual men.
“Monkeypox is not a sexually transmitted infection in the typical sense, but it can be transmitted during sexual and intimate contact as well as with personal contact and shared bedding and clothing.
“Anyone can spread monkeypox through contact with body fluids, monkeypox sores or respiratory droplets when close to someone.”
He urged anyone with an unexplained rash other symptoms to seek medical attention.
“Remind the health care provider caring for you that this disease is being observed in other parts of the world right now with a notable fraction of cases occurring among gay men,” Brooks said. “Importantly, don’t hesitate to advocate for your health and inform your doctor of your concerns if you think you might have been exposed.
“In some cases during the early stages of illness, the rash has been mostly in the genital and perianal areas.”
In some cases, it can cause anal or genital lesions that look like other diseases such as herpes, chickenpox and syphilis.
Is there a treatment for monkeypox?
Because the monkeypox and smallpox viruses are related, the tools used to tame smallpox outbreaks in the past can be used in response to monkeypox outbreaks.
There are two vaccines and one antiviral drug that are approved by the U.S. Food and Drug Administration to use against smallpox. One of those vaccines, Jynneos, can be used after exposure to monkeypox to prevent illness or make it less severe in people ages 18 and older.
However, the CDC says the sooner the Jynneos vaccine is given after exposure, the better. Ideally, a person who was exposed to monkeypox should get vaccinated within four days of exposure to prevent disease or four to 14 days after exposure to limit severity of disease.
“We’re working now to develop recommendations to ensure that the vaccine supplies that we have are available to those who need it, and that doctors can use it to decide what’s right for their patients,” McQuiston said.
In addition, states and U.S. territories may request doses of the ACAM2000 vaccine, which is FDA-approved for protection against smallpox and believed to also protect against monkeypox.
However, ACAM2000 cannot be given to anyone who is immunocompromised or to people with heart disease. It also is more likely to cause serious side effects.
How can I get a vaccine/get tested?
While the CDC does not advise widespread monkeypox vaccination, it suggests the vaccine may be recommended for people who:
- Have had confirmed close physical contact with someone diagnosed with monkeypox.
- Have a sexual partner who was diagnosed with the virus.
- May have been exposed.
- Are men who have sex with men who have recently had multiple sex partners in an area where there was known to be monkeypox or where the virus was spreading.
- Perform laboratory testing to diagnose monkeypox and may be at risk of exposure,
More of the two-dose Jynneos vaccines are being distributed to states to help combat the outbreak. So far, the U.S. Department of Health and Human Services has allocated 9,000 doses of vaccine and 300 courses of antiviral smallpox treatments from the Strategic National Stockpile to 32 states and U.S. territories. The goal is to distribute 1.6 million doses over the next several months.
Federal officials also are ramping up testing capacity — providing orthopoxvirus tests to 78 sites in 48 states, allowing the U.S. to conduct 10,000 tests per week.
The CDC recommends that anyone with a rash that is consistent with monkeypox should seek medical care.
The agency also is urging health care providers to be on the lookout for possible cases, regardless of a patient’s risk factors, travel history, gender or sexual orientation.
Is traveling risky because of monkeypox?
Though the risk to the general public is low, the CDC issued a Level 2 travel alert in May urging people to “practice enhanced precautions” because of monkeypox infections spreading globally.
Those precautions include avoiding:
- Close contact with sick people — including people with skin or genital lesions, and contact with materials used by sick people or animals, such as clothing, bedding or health care materials.
- Contact with dead or live animals such as small mammals, including rodents like rats or squirrels and nonhuman primates such as monkeys and apes.
- Eating or preparing wild game meat or using products that come from wild animals from Africa, such as creams, powders and lotions.
The virus has been identified in the following 51 countries: Argentina, Australia, Austria, Bahamas, Belgium, Benin Brazil, Bulgaria, Canada, Chile, Colombia, Croatia, Czechia, Denmark, Estonia, Finland, France, Georgia, Germany, Gibraltar, Greece, Hungary, Iceland, Ireland, Israel, Italy, Latvia, Lebanon, Luxembourg, Malta, Mexico, Morocco, Netherlands, Norway, Peru, Poland, Portugal, Romania, Serbia, Singapore, Slovenia, South Africa, South Korea, Spain, Sweden, Switzerland, Taiwan, United States, the United Arab Emirates, the United Kingdom and Venezuela, according to the CDC.
Could monkeypox become endemic in the U.S.?
Some scientists have speculated that monkeypox could become a more common disease in the U.S., where there is a constant, baseline level of spread, as there is now in parts of central and western Africa.
McQuiston detailed the CDC’s strategy to prevent that from happening:
“We’re working very hard to contain it,” she said. “In the United States, our containment strategy is focused on identifying cases, identifying their contacts and making sure they get vaccine offered to them, and that … cases are being isolated to prevent onward spread.
“I think it’s too early to know whether monkeypox could become endemic but I think it’s important to keep in mind that monkeypox has been endemic in several countries for decades.”
Have monkeypox cases been reported in the U.S. before?
Yes. Last year, two separate cases were confirmed in Texas and Maryland in people who had returned from Nigeria.
And in 2003, an outbreak occurred in six states — Illinois, Indiana, Kansas, Missouri, Ohio and Wisconsin — when 47 people were infected with monkeypox after coming into contact with pet prairie dogs. The pets had previously been housed near small mammals imported from Ghana that were infected with the virus.
Contact Kristen Jordan Shamus: kshamus@freepress.com. Follow her on Twitter @kristenshamus.
Subscribe to the Free Press.


















Discussion about this post