Blood clotting, also called coagulation, is a vital process the body uses after an injury to stop bleeding and help prevent infections. But sometimes, blood clots form inside an artery or vein, where they can cause damage or even lead to death.
So what causes blood clots? And what makes them more likely to form?
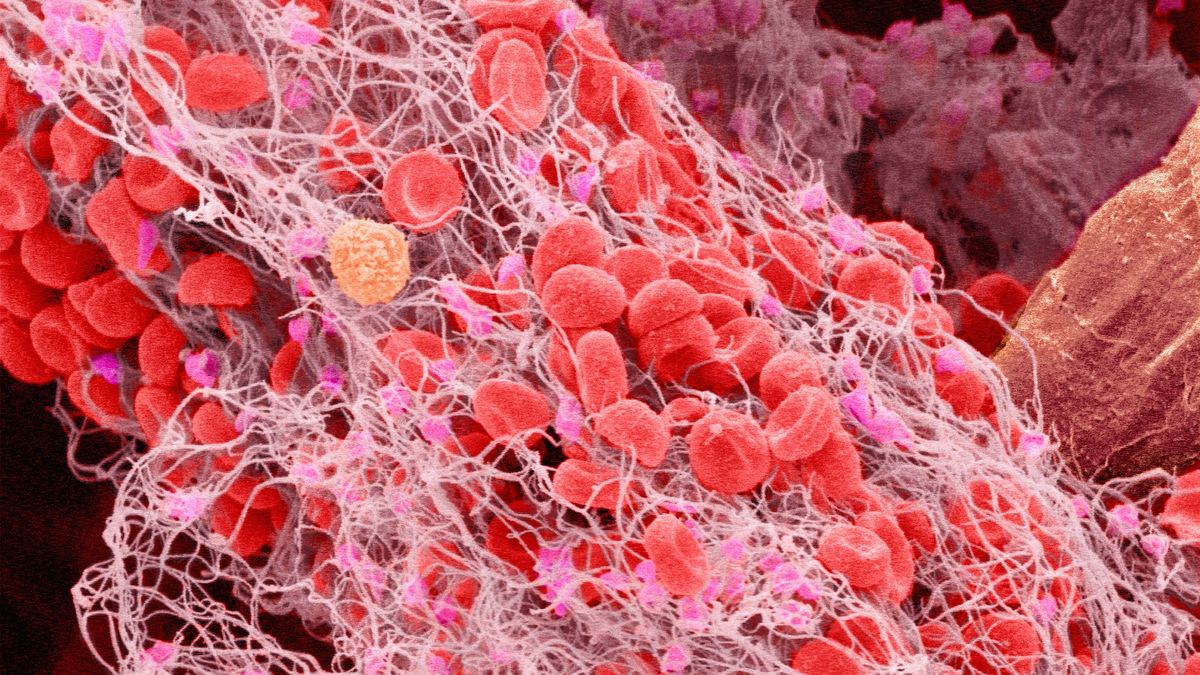
A blood clot can form when a blood vessel is injured. This kicks off a chain of events that causes a protein called thrombin to accumulate nearby. The thrombin then activates bits of cells called platelets in the blood, causing them to form a plug that covers the injury site.
These platelets also bind fibrinogen, another bloodborne protein. Thrombin converts this fibrinogen into a tough protein called fibrin, which forms a mesh that bridges the platelets to reinforce the plug. Once the wound has healed, these clots dissolve.
Related: What’s the rarest blood type?
In some cases, though, blood clots can form when there isn’t an acute injury. This happens when factors in the blood make it more likely to clot; blood vessel linings are damaged over time by disease; or blood flow is restricted, for example, by plaque buildup caused by coronary artery disease.
Medically known as a thrombus, a blood clot that forms in one of these ways may stay in the blood vessel without dissolving and block the passage of blood. This can cause tissue damage if the clot cuts off blood flow completely. If thrombi form in the heart, they can lead to heart attacks. If they form in the brain, they can cause stroke.
If some or all of the clot breaks loose from its original site, it is called an embolus. Broadly, emboli are masses that travel through the bloodstream and can get stuck if they reach a vessel that’s too narrow.
Such roving clots are especially dangerous because they can travel to any part of the body. In a condition called deep vein thrombosis (DVT), a clot forms in a large vein, often in the legs, and can break off and travel to the lungs. That is then called a pulmonary embolism, which is a life-threatening medical emergency.
“I cannot stress how important it is to recognize the symptoms of a blood clot,” Dr. Rachel Rosovsky, director of thrombosis research in the Division of Hematology at Massachusetts General Hospital, told Live Science. “If you have a DVT, it could be leg pain, redness or swelling. For a pulmonary embolism, it could be chest pain, pressure, shortness of breath or a fast heart rate.”
It’s important not to ignore these symptoms, especially if you are at risk of a blood clot, because a successful recovery often depends on quick treatment.
Some diseases make blood more likely to clot. There are genetic conditions that increase the levels of clotting proteins in the blood; reduce the levels of proteins that prevent or dissolve clots; or otherwise impair those proteins’ functions.
Other conditions — including cancer, autoimmune diseases, high blood pressure and infections like COVID-19 — may also throw off the body’s delicate balance of coagulation factors. In COVID-19, a combination of excessive inflammation and rogue antibodies are thought to increase the blood’s propensity to clot.
Related: If blood is red, why do veins look bluish?
Both pregnancy and hormonal treatments, such as some forms of birth control and hormone replacement therapies, are tied to an increased risk of blood clots. Research suggests that anxiety and depression may boost the risk of DVT by increasing stress-related neural activity tied to clot formation.
Lifestyle factors also contribute to a person’s risk of blood clots. Smoking raises the risk by increasing inflammation in the body and making platelets more reactive. Obesity is also tied to a higher risk of blood clots; this may be partly because signaling molecules made by fat cells can boost levels of clotting factors and make platelets stickier.
By limiting a person’s mobility, long-haul travel, injuries such as bone fractures, and major surgeries can all temporarily increase the risk of dangerous clots. That’s because less movement means less blood flow, more inflammation and more activation of clotting factors in response to that inflammation.
Some of these risk factors can be mitigated, though.
“If you sit at a desk all day, get up and walk around every hour,” Rosovsky said, adding that seated travelers should wear compression stockings or take regular movement breaks during their journeys. She also recommended that, in general, people stay well hydrated, maintain a healthy weight, engage in physical activity and avoid smoking.
“Right now, someone dies of a blood clot every six minutes,” Rosovsky said. As many as 100,000 die of blood clots each year in the U.S. Rosovsky stressed that it’s important to know your risk factors and how to mitigate them, but also, to be aware of the signs and symptoms of blood clots and seek medical attention if you experience them.
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line “Health Desk Q,” and you may see your question answered on the website!



















Discussion about this post