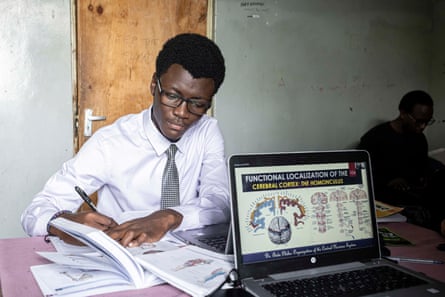
Scalpel in hand, Carl Mwangi, a first-year medical student at the University of Nairobi, slices through the brain tissue. “To figure out where the vessels are, you have to dig in deeper,” he says, excited to be dissecting a human brain for the first time. But if he wants to do more dissections, the aspiring neurosurgeon will have to secure one of only 10 places on the anatomy programme here.
Only postgraduate students and those specialising in anatomy are able to get hands-on dissection experience as Kenya’s oldest medical school grapples with a shortage of cadavers. Until recently, medical students would spend at least 250 hours on dissection in their first year. However, most students now learn through prosection – examining bodies that have already been cut open. Up to 12 students have to learn using one cadaver in anatomy class.
“Undergraduates’ exposure [to dissections] has reduced drastically,” says Musa Misiani, an anatomy tutor at the university, who is concerned how this will affect future teaching.
More medical schools – Kenya now has 12 – and higher enrolment rates have increased demand for cadavers. These are mainly sourced from morgues, which can hand over bodies if they have not been claimed after 21 days and efforts have been made to contact relatives.
Nairobi university has a body donation programme but has only received two to three annually over the last five years. Awareness of the programme is low, even among medical students.
“Accessing the bodies through traditional means is becoming more of a challenge,” says Prof Moses Obimbo, head of the human anatomy department. “We need to inform our people of the importance of body donation. We try to be innovative but if we run out of these resources to train, and one of the key resources is cadavers, I foresee a fall in standards of medical school training.”

It’s not a new challenge for the school. When it first opened in 1967, founder Joseph Mungai had to source corpses from a medical school in neighbouring Uganda. But the situation is now serious, and speaks to a wider issue about attitudes in Kenya towards donating bodies and organs to science .
A 2016 study of students at the university showed that while surgical trainees and medical students would recommend people donate their bodies to science, nearly 50% are not inclined to do so themselves, citing cultural and religious reasons. Some feared their bodies would be excessively mutilated or mishandled.

A wider study that included other Kenyan medical schools found that even among those willing to donate follow-through can vary. Potential donors don’t always sign a donation card or include the bequest in their will. Family members have contested bequests to the University of Nairobi. “We live in a cultural context, and people in Kenya want to bury their dead,” says Misiani. “That’s one of the biggest barriers.”
To encourage more donations while taking on board people’s sensitivities, the university has started conducting burials for cadavers after they’ve been used. Last year, it held its first memorial service for body donors.
Morticians say medical schools could do more to source bodies. A more formal arrangement could be made between mortuaries and medical schools. About 100 unclaimed bodies from Mbagathi hospital in Nairobi were buried last year but could have been used for research.

After having a front row seat on health emergencies, Philip Ogola, 46, a former humanitarian worker from Nairobi, wants to donate his body or his organs to science. “You see people appealing for blood, bone marrow, eyes,” he says, but even though the need is dire, there’s often no response to public appeals, except for those made by prominent people. “It made me wonder: why do people only donate when there’s a disaster? As a country, we don’t have a donation culture.”
Medics say the country is also in urgent need of organ donors with a significant number of patients dying each year because they can’t find a match.
Ogola’s family are not pleased with his decision to donate. “Why does he want to do that when he knows our traditions?” asks his mother, Angelina Awinom, his next of kin. “I’ve had so many thoughts since I found out about it. Where would his body be taken and what would be done with it? It has caused me a lot of grief.”
The decision, she said, would be an unwelcome surprise to relatives and friends in their village in Siaya, western Kenya, where burial traditions hold particular importance, and a number of rites call for an intact body. Awinom, a practising Christian, is unsure if she will respect her son’s wishes if the time comes. “Even if I do it, it will not be with a willing heart,” she says.

Ogola is due to have a cornea transplant at Lions SightFirst Eye hospital, a private facility in the city. About 1,000 people are on the waiting list. The hospital receives an average of 15 cornea donations a month, and now mostly relies on local donations.
Christopher Mwangala, the hospital’s eye bank coordinator, would like Kenya to make organ donation the legal default at death – unless a person opts out – to increase donor numbers and save, or improve, many lives. Similar policies have been adopted in countries across the world, despite some debate on the efficacy of the opt-out system.
“That’s the only way we can get donations,” says Mwangala. “Culture is hard to break.”
Late last year, Kenya launched the Tissue and Transplant Authority – replacing the health ministry’s previous department – to encourage donations through regulations that protect organ donors and recipients. It also aims to make organ transplants – still largely a preserve of the privileged – more accessible.

Poor regulation has allowed room for an illicit trade in organs , which the authority hopes to curb. Officials admit they are “playing catch-up” and have much work to do. “We are coming into an environment where we are regulating what’s already being practised,” says Alfred Obengo, chair of the authority.
Medical students say they are not learning enough about organ donations and transplants. Only about 3% of students felt confident in their knowledge on the subject, and less than 10% were familiar with the country’s transplant laws.
Ogola does not plan to change his mind about donation. “We need to normalise these conversations,” he says. “It’s the only way to end the stigma.”


















Discussion about this post